March 6, 2020 by John Fernandez
Big Advances for the Tiniest Patients

In our modern world of digital photography and social media, very few people have not encountered a photo or video of tiny babies born into the world way before their mother’s nine months of pregnancy concluded. While heart-wrenching to see, these tiny babies are making great strides to survive and thrive, thanks to advances in neonatal medicine.
 Babies born before 37 weeks gestation are considered preterm or premature, according to the March of Dimes. The Centers for Disease Control and Prevention (CDC) reports that 500,000, or 1 in 8, babies are born premature each year in the United States. And, the CDC says, preterm birth accounted for about 35 percent of infant deaths in 2009, more than any other cause. Yet a Swedish study published in the June 3, 2009 edition of the Journal of the American Medical Association showed that babies born at 23 weeks now have a greater than 53 percent chance of survival because of advances in perinatal and neonatal care.
Babies born before 37 weeks gestation are considered preterm or premature, according to the March of Dimes. The Centers for Disease Control and Prevention (CDC) reports that 500,000, or 1 in 8, babies are born premature each year in the United States. And, the CDC says, preterm birth accounted for about 35 percent of infant deaths in 2009, more than any other cause. Yet a Swedish study published in the June 3, 2009 edition of the Journal of the American Medical Association showed that babies born at 23 weeks now have a greater than 53 percent chance of survival because of advances in perinatal and neonatal care.
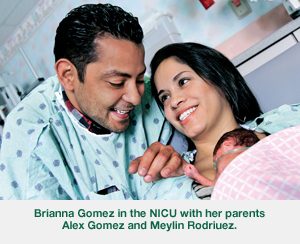
Babies like Brianna Gomez who was born earlier this year at Baptist Hospital at just 23 weeks gestation and weighing about 1 pound. Instead of cutting her umbilical cord immediately, her medical team allowed blood to flow from the mother’s placenta to the baby for an extra 30 seconds or so. This 30- to 60-second delay in umbilical cord clamping — recently endorsed by the American College of Obstetricians and Gynecologists and being performed by doctors at Baptist and South Miami Hospital during deliveries at 32 weeks and earlier — helped Brianna avoid many of the complications common in such tiny newborns.
“Higher blood volume decreases the risk of brain hemorrhage, lessens the need for blood transfusions and helps stabilize blood pressure,” said Andrew Kairalla, M.D., medical director of neonatology at Baptist Children’s Hospital. “This is a very exciting and dramatic advance in the treatment of very premature infants.”
“In the past decade, we’ve made major improvements in treating a preemie for respiratory, heart and kidney problems,” said Jorge Perez, M.D., medical director of neonatology at South Miami Hospital’s Center for Women & Infants. “But when you have low blood volume, the vital organs, including the brain, are not getting enough blood flow or oxygen. Until now, we had no control over what was happening in the brain. It was devastating. But the higher blood volume seems to protect the brain.”
Other Advances
Obstetricians and pediatric neonatologists at South Miami and Baptist Hospitals also are working on a number of other new techniques to help preemies. These include drawing blood from the mother’s placenta instead of the baby for the first necessary lab tests, again reducing the need for a blood transfusion. And doctors at Baptist Hospital, in some very specific emergency deliveries, are performing umbilical cord milking or stripping, where blood is pushed through the umbilical cord to get extra blood volume to the baby even faster than through delayed clamping. Both hospitals, too, are using neonatal therapeutic hypothermia to prevent permanent brain damage caused when babies’ brains are deprived of blood and oxygen during their birth, leading to a potentially deadly condition known as hypoxic ischemic encephalopathy.
South Miami Hospital’s care of premature babies recently received the Gold Seal of Approval by The Joint Commission, which holds hospitals to high standards for performance and safety.
While methods for treating preemies continue to improve, Brianna, and other babies who spent prolonged periods of time in the NICUs at South Miami and Baptist Hospitals reunite with their doctors and nurses each year at annual reunions hosted by each of the hospitals.
“We’re continuously in search of therapies that help these babies,” Dr. Perez said. “The advancements we’ve made over the last five years even, have helped these tiny babies not only survive, but thrive.”
top stories












There are no comments